Medice, cura te ipsum*
Sounds to me like it will be expensive and probably difficult to treat
As a younger physician, I would frequently complain that my medical training had seemingly failed or at least misdirected me, not altogether different from my first long motorcycle ride. I had excelled in the safety course and done everything I was supposed to do to prepare, but nearly put the shiny side down on my first really curvy road.
That is, until I figured out that school was simply for developing tools I would need to tackle whatever new, rare, different or complex situations might come at me.
Motorcycling the wide variety of curvy roads became an interest, and no longer a fear. It was about the same time in my life that I looked at my office bookshelves jammed with medical texts and realized those were also just tools in my bag. The proverbial “textbook case” is quite unusual, but rarely follow the textbook case on further inspection.
Always use the right tool. My current dream – Zero’s DSR-X
Sadly, that is the Western perspective of medicine. In school, the human body is parsed into systems to master, and theoretically we then reassemble them into the whole. Reassembly is mostly on your own however, if you even understand the concept. Without the appreciation for the whole, what good is mastery of a system that will only rarely present itself so refined?
Many people and other physicians have asked me why in the world I would ever choose to specialize in Oncology. For years I thought to myself and replied that what interested me most about Oncology was the ability to help people at a particularly difficult part of their life while also requiring complicated sciences to do that well. While that’s all true, a better explanation thankfully occurred to me later.
Cardiology, Nephrology, Neurology, Pulmonology, Gastroenterology, etc., are centered around an organ system. It was becoming increasingly obvious to me that the better specialists were always those who also looked outside their immediate system for answers. But wait, you say, Oncology is not an organ at all! Bingo. Between the diseases and the therapies, no system gets special treatment, and no stone goes unturned. That’s my kind of riddle.
Basically, there are two types of people. Those who can extrapolate
Even psychiatry is somewhat taught as a stand-alone system, though there is the ever present caveat to “first exclude organic causes,” that is to say make sure there are no measurable changes in organs or tissues to explain the symptoms, e.g. syphilis, multiple sclerosis, heavy metal toxicity, Parkinson disease, Alzheimer disease, AIDS, and more recently, Covid-19.
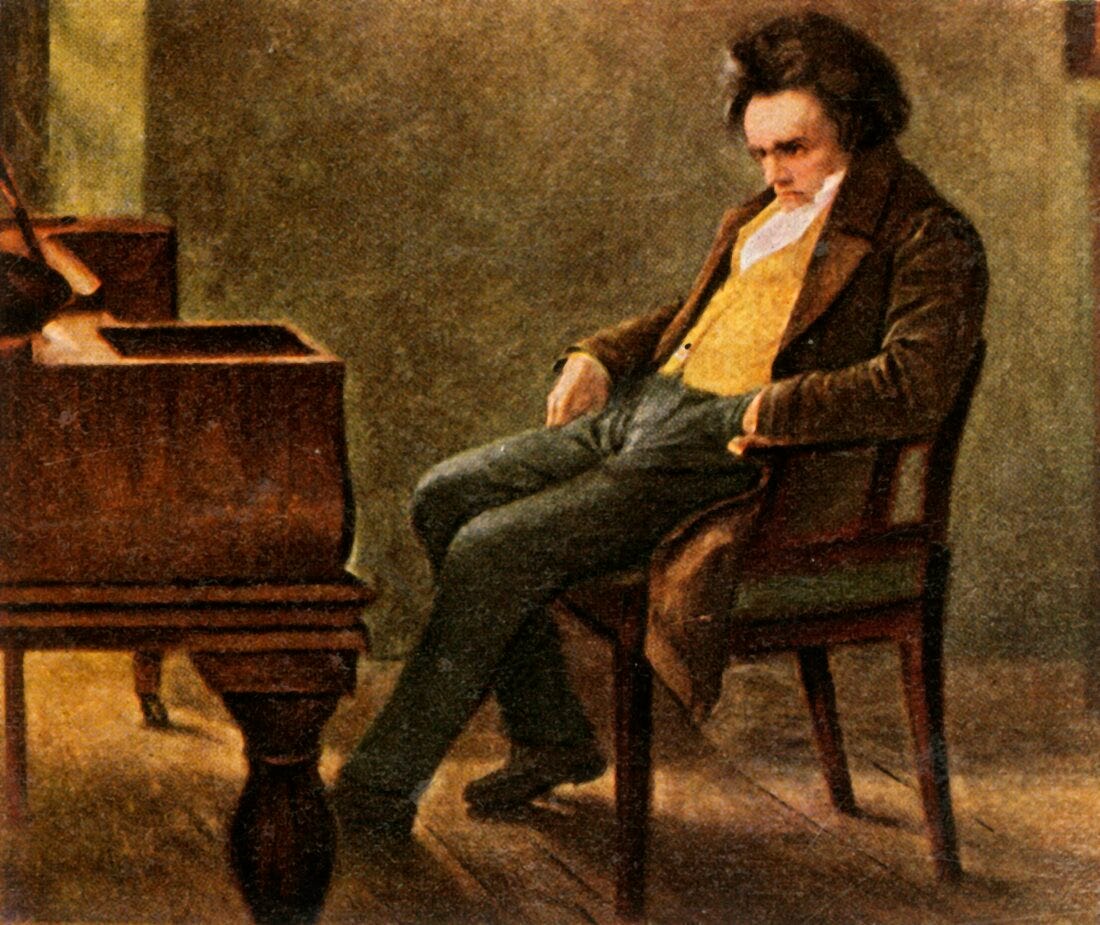
Ludwig van Beethoven, one of the pioneering heavy metal composers (his hair was found to have very high lead levels, but he also appears to have had Hepatitis B infection)
I am ever thankful that in my residency, our Psychiatry Department taught Consult-Liaison Psychiatry (C-L Psychiatry), also known as Consultative Psychiatry or Consultation-Liaison Psychiatry. It is a collaborative, holistic approach to psychiatry. In my biased opinion, that is the only way psychiatry should be done, not to mention the only way effective psychiatry can be done.
Most of Psychiatry does not agree however and considers C-L Psychiatry as a “branch” of Psychiatry. Oh. The majority of the profession comfortably excludes the rest of medicine in their own little gated community, dysfunctionally triangulating their patients with the patient’s other providers. So I am also disappointed I had that medical upbringing, well, because I was led to expect it.
I did not go into Oncology because I have it.
So I’m still ruminating over a 2013 article I read from the Yale Journal of Biology and Medicine (No, that’s not on my list of frequently read journals. It may even be the singular article I’ve read from that niche Journal.)
The author laments that “the bulk of mental health services for people with depression are provided in primary care settings. Primary care providers prescribe 79% of antidepressant medications and see 60% of people being treated for depression in the United States, and they do that with little support from specialist services. Depression is not effectively managed in the primary care setting...” and so forth.
When you only have a hammer, everything looks like a nail.
That there is little support from mental health specialist services is quite the understatement. Good luck trying to get someone to a psychiatrist or other mental health provider, even for the worst of cases. The sordid experiences of being blocked at almost every turn is exhausting, and in some extreme cases has in my opinion led to several suicides of which I’m aware. So, no, I’m not surprised that the author had so little introspection to criticize the rest of us trying to do our best with what little we have.
It is fairly standard practice that mental health providers themselves benefit from therapy and they are encouraged to do so. “Compassion fatigue”or “therapist burnout” can also result in insomnia, anxiety and depression for the mental health provider.
But as a victim of their manufactured exclusive community and what I consider to be the chief perpetuation of the stigma of mental health, it is not uncommon for psychiatrists to unwisely and unprofessionally treat themselves for mild to even severe depression. Sigh. Again with that complete lack of introspection and exceptionalism. So is it really that much of a surprise that psychiatrists, and physicians in general have the highest rates of suicide of any profession?
Now permit me to close that loop. If primary care providers prescribe 79% of antidepressant medications and see 60% of people being treated for depression in the U.S., are primary care providers allowed the same possibility of “compassion fatigue” or “therapist burnout”? Are primary care providers also able or even encouraged to routinely access therapists for themselves?
I can answer that with a resounding hahaha followed by no, it’s not even on the national radar.
Normal tourist visit of our Nation’s Capitol
I must admit that one of the biggest reasons I had hope for the Harris/Walz ticket was purely selfish. I had hoped that vast majority of my patients would then be less anxious and less depressed. In 2021, it was estimated that the stress of 2020 was the catalyst for one out of six Americans to begin therapy for the first time.
My best guess is that like many businesses which went under in 2020, many people were already struggling and 2020 was the last straw for them. Like so many self-reported health statistics, if one out of six recognize this problem, the actual incidence is more than likely at least double that.
Along those lines, and what I still consider pertinent to current events, I want to leave you with a vignette I’ll never forget.
I was working at Kaiser, a system notorious for obstructing patients’ messages to their providers. I gave each of my patients of my direct number and some instructions — they were never to leave time-sensitive messages and should leave the message as soon as the concern occurred to them with their contact info, and I would listen to their message the next morning and get back to them as soon as possible. Voicemails were time-stamped.
One usual morning a message played from 1 a.m. “I see blood. It’s everywhere. I smell blood. It’s all around me. It’s awful.”
The caller did not leave a name or contact info, but I recognized her voice immediately though it sounded somewhat flat this time. She was an elderly, retired Army nurse, and she and I often talked about the military as I had been a Navy/Marine Corps physician. She had also previously told me that as a young nurse she was one of the first military medical responders to enter a liberated Nazi concentration camp.
I called her at home and she confirmed having left the message. She was clearly shaken and not herself. I asked her if she was safe, “yes,” or if she might be suicidal, “no,” and told her I would call her right back.
I immediately called our Psychiatry Department and asked for an urgent appointment and why. I was told to send the referral, and she would be seen “in a couple of weeks.”
I then called the one Psychiatrist in the same department that I knew had compassion and ethics, and she said, “Send her up.” I called my patient at home with that plan, she was seen that day, and I have absolute certainty to this day that she was helped and a crisis averted.
That, folks, is a textbook case of Post-Traumatic Stress Disorder (PTSD).
Though we are getting better at recognizing PTSD, our ability to address it effectively remains poor. The best approach to PTSD is to stop creating situations that cause it, and no that’s not just war.
Yes, I’m afraid we’re looking at a whole new round of PTSD, and worse, I’m afraid that providers around the country already have compassion fatigue from the past 8+ years.
Please take care of yourself and one another and if you have the suspicion someone needs more help, I sure hope you can find it.
Here’s two nationwide resources:
Call 988, the three-digit, nationwide phone number to connect directly to the 988 Suicide and Crisis Lifeline
Text HOME to 741741 to reach a live volunteer Crisis Counselor.
*Medice, cura te ipsum, or Physician, heal thyself.
Though most commonly attributed to a quote from Jesus in Luke 4:23, at the time it was generally intended to criticize hypocrisy.







Damn! I like you a lot. I wish there were more physicians like you around. I have never understood why the medical profession focuses on stand alone body systems. Even to this fairly well educated but not in the medical world person, it makes sense that there would be impact and overlap. I guess we have all these specialities b/c we are a departmentalized society. We don't see things as part of a whole. Each body system (and each gov't system, etc) stands alone. I'm not adverse to Western medicine but it sure has its limitations, as it is currently generally practiced.
And speaking from personal experience, you are so right about the mental health issues you bring up. My primary care provider called me on some words/behaviors some years ago and offered meds to me b/c that was all she could offer. Later, I saw the need for more help and found myself a psychiatrist BUT I could afford that. I needed more than meds and I had the money. NOT right. Money gets in the way. Did the psychiatrist ever really question my physical health? Sometimes but always rather vaguely. I will add that he was willing to work with me with meds but he also respected and valued my desire to avoid medication if I could. Things got dicey from time to time but we worked through it.
I do appreciate your columns. You give me a lot to think about.
Do you still ride the motorcycle? There are beautiful roads in NorCal. Watch out for the idiot drivers.
I’m a clinical psychologist, but I have an unusual degree, a DMH, which stands for Doctorate in Mental Health. I got my masters degree in two years at UC Berkeley and my classes were primarily physical health. Class is such as anatomy, physiology, neurology, pharmacology, etc. our professors believe that a good grounding in the physical sciences would make for a better mental health professional, and they were right. I then became a behavior medicine consultant at Kaiser. Although I was extremely well qualified to work with medical doctors because of my educational background I never received the administrative help that I needed. What I noticed is exactly what Dr. Rochat is talking about, the people in psychiatry, never wanted to talk to the medical doctors who were referring patients to them. I would attend, when I was in the psychiatry department, grand rounds once a week and they very often evolved into psychiatrist, making fun of medical doctors and their “absurd and unnecessary“ referrals whenever I received a referral from a medical doctor. I immediately contacted that doctor got more information and scheduled an appointment for the patient within a week. It is possible to do that. One of the reasons psychiatry says they have two grade a patient load is that they attend to damn many meetings! I actually loved working with the medical doctors in the family practice clinic and feel that I could be helpful and that I was appreciated, something I never felt when I worked in the psychiatry department